Spatially Fractionated Radiation Therapy
A look at the history, approaches, and new research of spatially fractionated radiation therapy.
Carbon Ion Therapy: a brief discussion of the pros and cons of the technology coming soon to the US
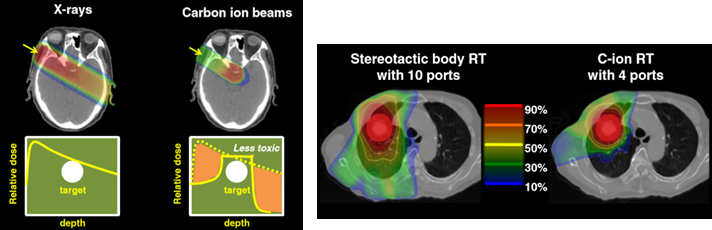
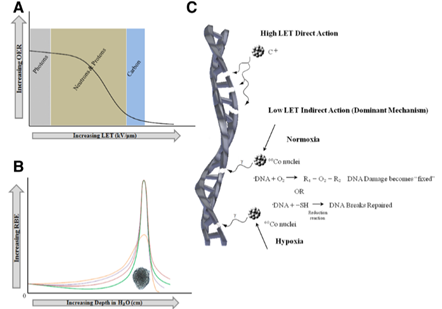
As in proton therapy, carbon ions demonstrate the Bragg peak phenomenon in tissue, with a majority of their energy being deposited at depth. This is especially advantageous in reducing the dose given to normal tissue beyond the tumor volume. Carbon ion beams also have a smaller lateral penumbra, which helps to limit dose to the surrounding tissue when compared to a typical photon beam.
From the radiobiological perspective, carbon ions confer a number of benefits:
These factors aid in the treatment of tumors that are typically identified as radioresistant. These combined radiobiological advantages result in more cell killing within the tumor and hence more tumor control. With higher RBE and LET, carbon ions increase cell killing compared to photon therapy to maximize tumor control while decreasing toxicity to normal tissue.
Clinical research has begun to reinforce the potential benefits of carbon ion therapy. In a trial for patients with bone and soft tissue sarcomas, good local tumor control was achieved, even in large and unresectable tumors. The boon here is that this subset of patients may not tolerate surgery or not qualify for surgery due to tumor size. At one year post-treatment, the local control rate was 88% and at three years, 71%. It was also found in these patients that there were relatively high survival rates: 82% at one year and 46% at three years post-treatment. In a different study involving bulky sacral chordoma tumors, results showed an 86% local control rate at five years and an overall survival rate of 88% at five years.
Schalff, et al. have compiled data comparing favorable clinical results using carbon ion therapy versus standard-of-care results for a number of treatment sites:
Despite the clear benefits of heavy-ion therapy, radiation therapy with carbon ions requires complex equipment, a synchrotron, and additional shielding. Building and maintaining the equipment needed is extremely expensive, approximately twice the cost of a proton facility, a drawback that has prevented investment in this treatment modality to date. So while carbon ion therapy has been shown in prospective trials and clinical outcomes to be effective for certain tumor types, there is still legitimate debate on the role it will play in the future of radiation therapy given the high barrier of entry and ongoing operation costs. With cost barriers for constructing new carbon ion facilities, there have been very few clinical trials that provide valuable clinical information for treatment options.
Carbon ion therapy is receiving recent attention for its potential role in cancer care. If ongoing clinical trials continue to show clinical benefit, it is possible that this technique will continue to gain traction, perhaps even within the United States. However, in spite of positive outcomes, the efficacy of carbon ion therapy must be such that the benefits outweigh the associated costs of construction, implementation, and maintenance of the technology.

After working with Radformation as part of an industry cooperative while pursuing her medical physics MS at Hofstra University, Carly now contributes to the AutoContour team as the Product Manger for AutoContour Models. In her free time she enjoys planning game nights with her friends and family.
Related tags: RadOnc News
A look at the history, approaches, and new research of spatially fractionated radiation therapy.
We’re taking a look at the abscopal effect, an antitumor effect at a location in the body distant to a radiation treatment site.
DIBH is a validated motion management technique that provides excellent dose coverage while sparing OARs.
Leave a comment