Radiation Oncology Accreditation: A Primer
Accreditation delivers clear value to radiation oncology departments via thorough practice assessment.
Final CMS ruling brings billing/reimbursement changes to departments nationwide starting January 2021.
*EDIT* Since the final ruling was initially reported, implications have been made by CMS staff that the model will be delayed until July 2021, along with other potential changes.
The episode-based approach is simpler on the surface: one bundled-payment for any 90-day course of treatment, with reimbursement rates dictated by the disease site. Earlier this year we summarized CMS’s proposed alternative payment model and its potential impact on departments nationwide. After receiving feedback from a number of professional societies and institutions, CMS crafted the final details for the test reimbursement model that goes into effect January 1, 2021. Mandated departments will have just three months between the final rule announcement and the model start date for implementation preparation.
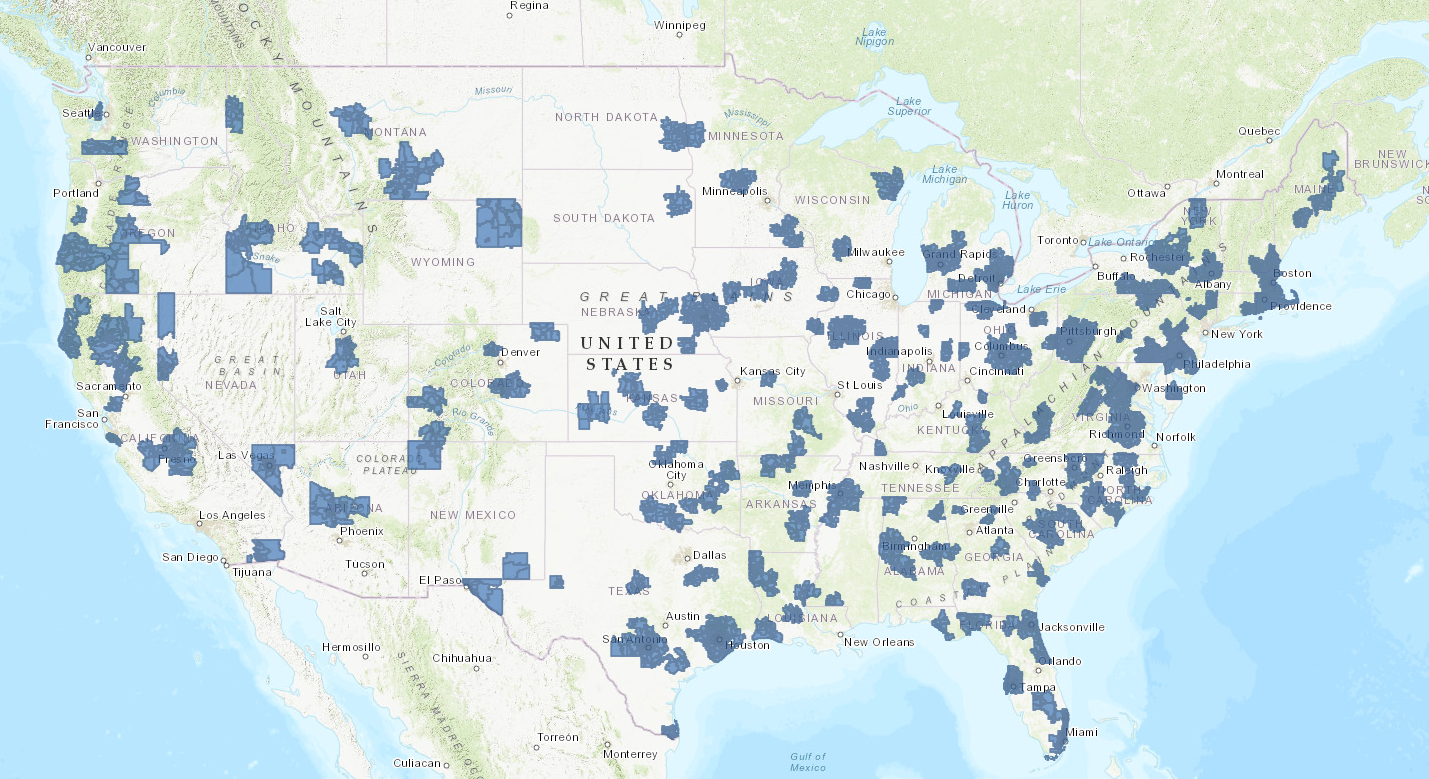
Most prominently, the number of clinics required for mandatory participation in the new payment system for medicare patients was reduced to 30% of departments in core-based statistical areas (CBSAs), down from 40% in the original proposal. Due to that and other factors, the total projected cost savings for CMS will be reduced from $260 million to $230 million over the course of the five-year trial period. Also contributing to the change in cost savings is a slight reduction to discount factors applied to base reimbursement rates. In an effort to reduce the financial burden on radiation oncology participants, both the technical (TC) and professional component (TC) discount factors were reduced by 0.25% to 4.75% and 3.75%, respectively.
Some special procedures were excluded from the model, including Y-90 embolization for liver cancer as recommended by ASTRO, as well as IORT treatments, which CMS determined is not a standard approach to treatment and may be misused if it were included in the model based on its low cost. Other exclusions include neutron beam treatment, electronic brachytherapy, and low-volume services, among others.
National base rates—from which department-specific reimbursement are derived—were augmented to incorporate more recent treatment cost data, as summarized below.
The resulting reimbursement payment to departments will be determined using the national base rates (see chart above) derived from weighted average of hospital-based claims data from 2016-2018. A number of modifiers are used to determine the final payout to each participant:
With a nationwide implementation, the effects will be broad, but could result in disparate effects depending on geography and patient makeup. According to ASTRO’s authoritative 37-page final ruling response to the final ruling, the society disagrees with CMS assertions that overall revenue impact will be <1% for most departments. Instead, they foresee a disproportionate burden in rural areas and small towns.
Though ASTRO is appreciative of the drop in the number of sites involved in mandatory model participation from 40% to 30%, they believe that the model ought to be voluntary, or at minimum include opt-outs for low census practices or exemptions for hardship (a tune many departments are whistling at the moment.) They suggest that implementing the final ruling in the middle of a global pandemic, with only weeks to prepare, may “foster unnecessary chaos and burden for the practices this model is designed to support.” To that end, ASTRO will continue working with Congress to create a realistic timeline for rollout of the model. The ACR has issued a statement of solidarity with ASTRO, committing to continued advocacy efforts.
On October 2nd, a coalition of ten professional societies, including AAPM, AAMD, and SROA, drafted a letter to CMS and HHS imploring the urgent consideration of a later implementation date of the final ruling, citing financial challenges in the COVID-19 environment. The signing groups make note of a genuine interest in a successful transition to value-based care, but claim that a 90-day implementation time from the time of final ruling release is “unrealistic under the best of circumstances.”
Other pertinent resources/links:
The philosophy behind the bundled payment model boils down to simpler, less confusing treatment reimbursement, and with CMS’ new RO-APM ruling being finalized, the episode-based model will finally see its start in radiation therapy departments nationwide. With the target being lower cost and higher quality care for patients, will the CMS RO-APM hit the mark?

Tyler is a board-certified medical physicist with extensive clinical experience in radiation therapy. He is active in the medphys community including several AAPM committees, the AAPM Board of Directors, and as an ABR orals examiner. Tyler dabbles in real estate investing, loves preparing breakfast for his three kiddos, and enjoys playing adult coed soccer.
Related tags: RadOnc News Compliance & Clinical Solutions
Accreditation delivers clear value to radiation oncology departments via thorough practice assessment.
Billing in RadOnc is a challenge, but innovative tools at our fingertips can streamline processes, reduce errors, and optimize financial viability.
We’ve all heard reports from colleagues about how radiation treatments sometimes just go wrong.
Leave a comment